Dental care in Australia is a hybrid marketplace with a public safety net. Children from eligible families receive significant support through the CDBS, enabling preventive visits and essential treatments at participating clinics. Adults who hold concession cards can access state and territory public dental services, though routine care may be prioritised below emergencies. For everyone else, private practices deliver the bulk of services, often financed through extras cover and out‑of‑pocket payments.
Cost pressures influence behaviour. When a scale and clean is postponed, biofilm matures, gingivitis advances, and restorative needs grow. Delayed treatment can turn a small occlusal filling into endodontics or extraction, with knock‑on effects for nutrition, speech, and confidence. Public waiting lists and provider shortages in some regions add friction, especially for those juggling shift work, child care, or long travel times.
Prevention strategies are well‑established. Fluoridated reticulated water supplies are a cornerstone, complemented by fluoride varnish programs for high‑risk children and fissure sealants for newly erupted molars. Clinicians increasingly apply risk‑based protocols: caries risk assessment, remineralisation plans, and recall intervals tailored to patient history. Tobacco cessation, alcohol moderation, and counselling around vaping and sugar exposure are now routine parts of chairside care.
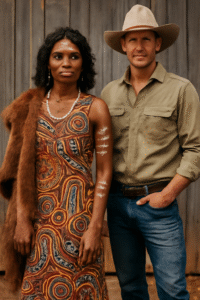
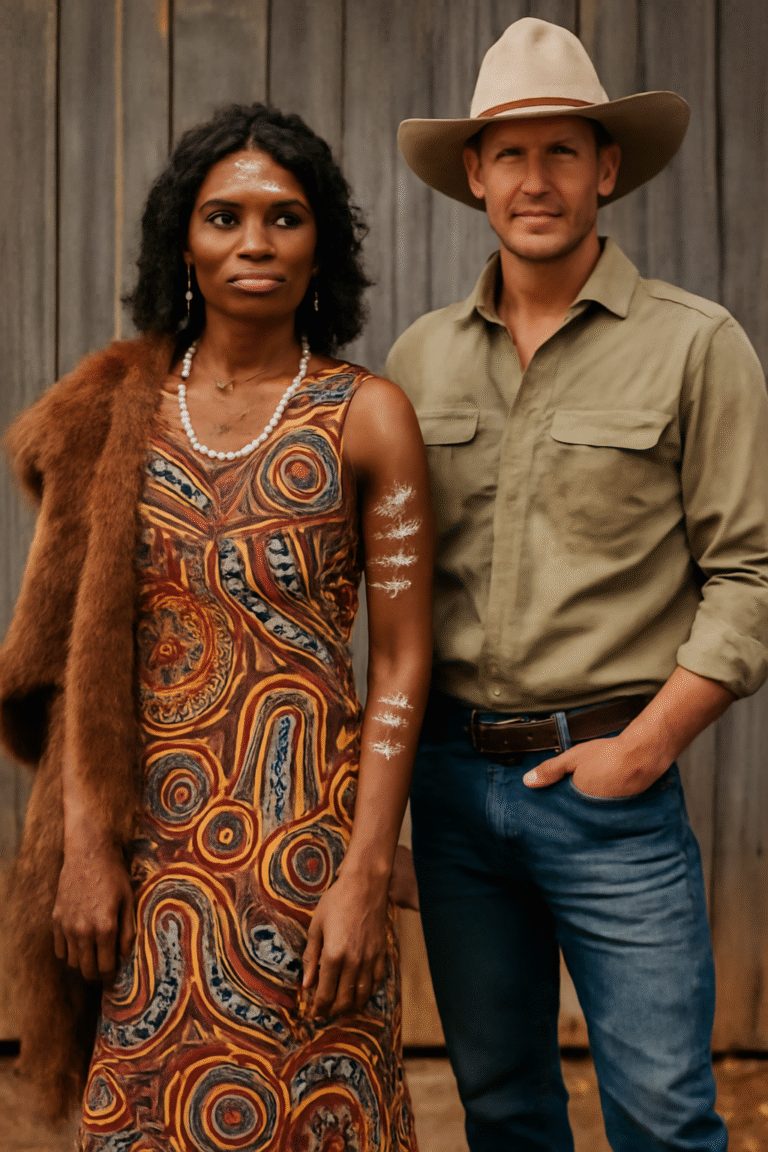
Communities with higher burden need tailored approaches. Aboriginal and Torres Strait Islander peoples benefit from culturally safe, co‑designed services that recognise community priorities. New arrivals and refugees may require trauma‑informed care and translated resources. People with disability often need longer appointments, desensitisation visits, or specialised equipment, which public clinics and certain private practices provide when properly funded.
Technology is narrowing distance. Remote consultations support urgent triage, informed consent discussions, and post‑op reviews. Portable X‑ray units and handheld intraoral cameras expand what outreach teams can achieve in schools, aged‑care facilities, and remote towns. In practice, digital workflows—from scanning to same‑day crowns—reduce visits and increase acceptance.
Financial navigation can make care achievable. Comparing gaps between providers, asking about payment plans, and timing treatment stages around insurance benefits can soften costs. Some practices belong to preferred provider networks that offer lower fees for covered items. Public clinics may offer priority pathways for urgent cases; staying reachable and responding quickly to appointment offers is crucial when on a wait list.
Australia is well‑placed to shift the balance from episodic fixes to lifelong oral wellness. If funding and innovation continue to focus on prevention and equity, fewer Australians will experience avoidable pain, and more will access the dignified, timely care they deserve.