Reducing obesity in Australia requires respectful, tiered care that matches support to need. Stigma and one‑size‑fits‑all advice can push people away from help, whereas structured pathways, cultural safety, and long‑term follow‑up improve outcomes.
Primary care is the anchor. Using the 5As framework—Ask, Assess, Advise, Agree, Assist—GPs start with weight‑neutral, behaviour‑focused conversations. They assess medical history, medications that may influence weight, sleep, mental health, and social determinants such as housing, transport, and food access. Team‑based care brings in dietitians, exercise physiologists, and psychologists, often under chronic disease management arrangements where eligibility applies.
Behaviour change works best with specificity: SMART goals, stimulus control at home, meal planning, and practical problem‑solving for high‑risk moments (night shift, travel, holidays). Telephone and digital coaching extend contact between appointments, offering nudges, relapse prevention, and peer support groups. For families, parenting programs that address sleep routines, fussy eating, and screen time can shift the whole household’s trajectory.
Pharmacotherapy and bariatric surgery have roles for some people with severe obesity and complications, but they are not first‑line and must be delivered in multidisciplinary pathways with informed consent and long‑term monitoring. Shared decision‑making is essential, as is proactive management of nutritional needs after surgery.
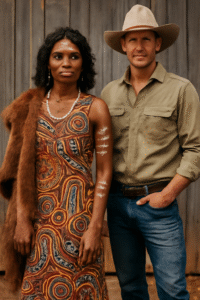
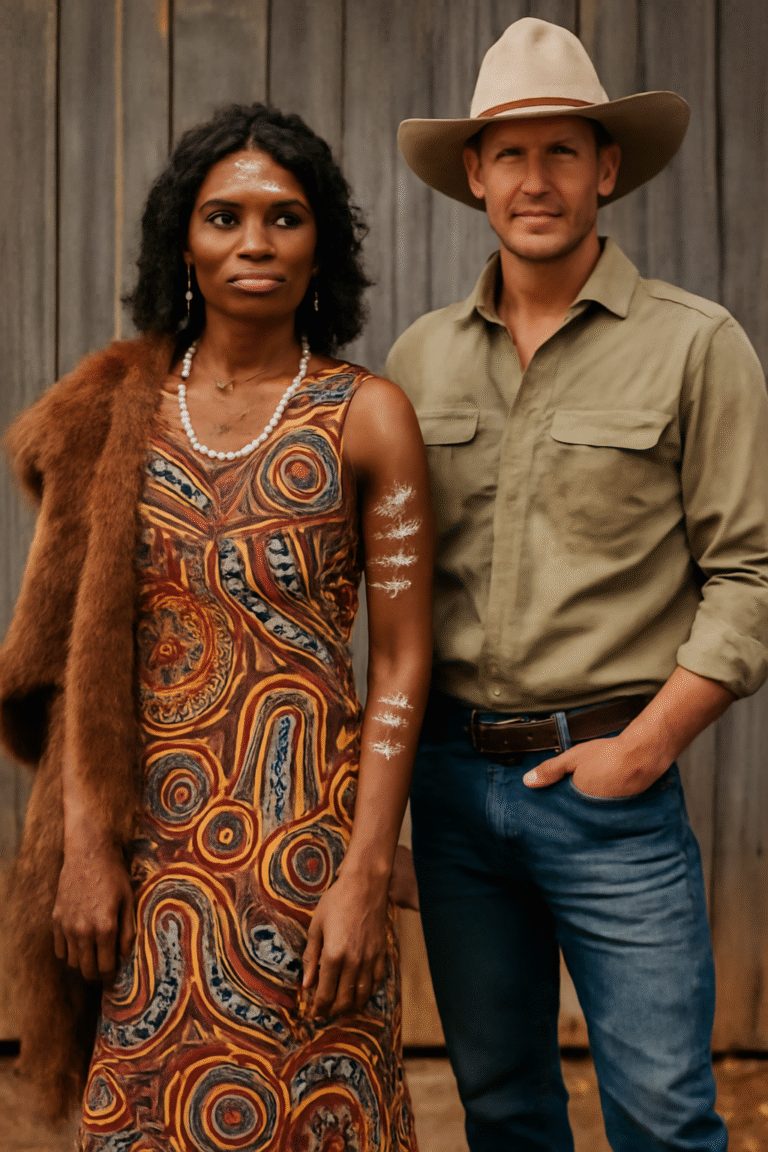
Cultural safety is non‑negotiable. Aboriginal Community Controlled Health Organisations provide holistic care that respects community priorities, integrates yarning and group programs, and addresses the wider determinants of health. For culturally and linguistically diverse communities, translated resources and bicultural workers can bridge trust and understanding.
Social prescribing connects people to non‑medical supports: community kitchens, walking groups, Men’s Sheds, community gardens, and financial counselling. Food insecurity undermines any nutrition plan, so linking patients to relief services, subsidised produce boxes, or healthy shopping vouchers can stabilise the basics. Housing and transport support may be the interventions that unlock healthier routines.
Clinics can adopt weight‑inclusive practices: private weigh‑in options, appropriately sized equipment and chairs, and training to counter bias. Metrics should extend beyond kilograms to include blood pressure, glucose control, fitness, sleep, mood, and quality of life. Success is multi‑dimensional.
Data closes the loop. Registries and audits track adherence and outcomes, enabling services to learn what works for whom. Telehealth expands reach to regional and remote areas when paired with local measurement hubs and outreach visits. Investing in care coordinators—especially for people juggling multiple conditions—prevents drop‑out and improves continuity.
By grounding care in empathy, evidence, and community partnerships, Australia can help individuals make changes that stick while narrowing inequities that have persisted for generations.